Keto Diet and Cholesterol: Everything You Need to Know
In a nutshell:
- Cholesterol is essential for our survival and has many different functions in our body.
- The fear of having high levels of (total) cholesterol is largely unfounded and there are other factors that are much more meaningful in determining the risk to develop heart disease.
- The first step of heart disease is not, as is often believed, cholesterol that is simply “clogging” the arteries but small injuries in our arteries where cholesterol can get trapped and build up.
- A carbohydrate-reduced diet has a positive influence on the most relevant risk factors for heart disease.
Cholesterol is absolutely vital for human life.
In fact, it is so important for us that almost every single cell in our body has the ability to produce it.
And yet it’s supposed to kill us at the same time.
The image of arteries clogged with cholesterol is very memorable and many people are justifiably afraid of eating themselves into a heart attack once they embark on the keto diet.
To add insult to injury, most physicians and nutrition experts warn us with a worried face of cholesterol and saturated fats from food and condemn the keto diet because of its’ higher fat content.
In this article, you will learn why the fear of a ketogenic diet in regards to your heart health is mostly unfounded and how it might even help to improve your most relevant heart disease risk factors.
The content provided in this post is for informational purposes only and does not constitute medical advice. It is not intended to replace professional medical advice, diagnosis, or treatment. See further information.
1. What is cholesterol?
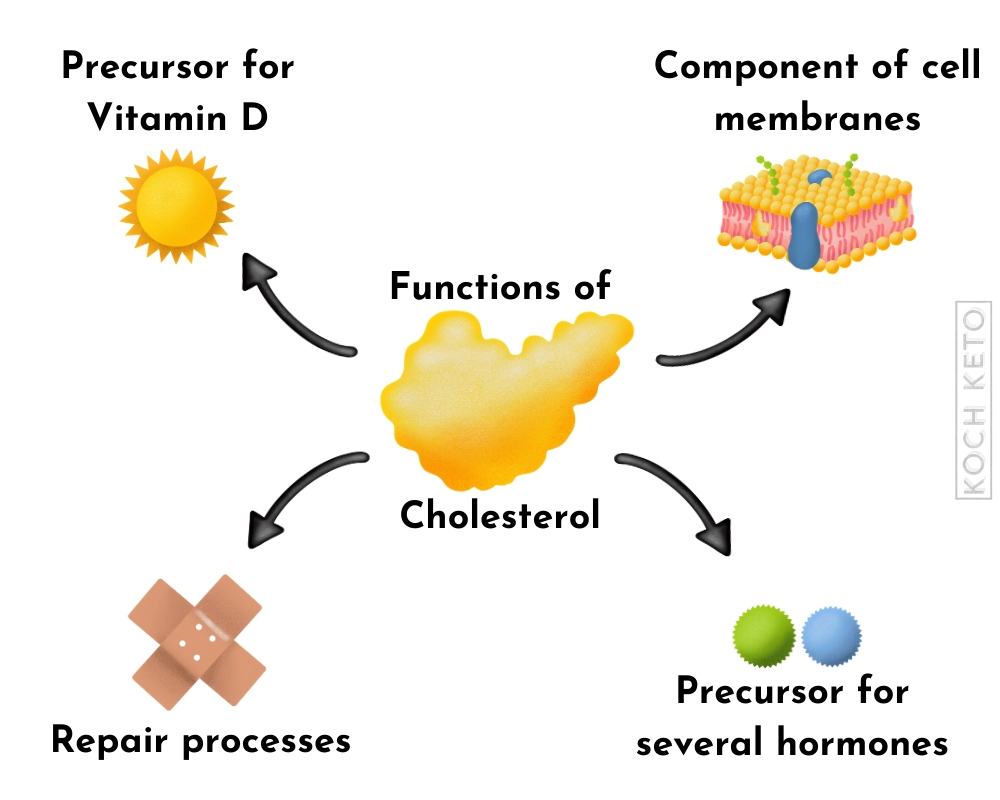
Cholesterol is a fat-like substance that has many different functions in our body.
It serves as a building block for our cell walls and is the precursor for many of our hormones as well as for vitamin D.
Insufficient levels of cholesterol can have a negative effect on our hormone balance as well as on our vitamin D level.
Cholesterol is also responsible to aid in repair processes in our body.
The majority of our cholesterol is produced by our own body
Cholesterol is so important for our body that almost all of our cells can make their own cholesterol.
Cells that cannot produce it on their own are supplied with cholesterol by transporter proteins.
In fact, our body produces so much cholesterol on its own that our diet only accounts for about 20% of our cholesterol levels.
In addition, our cholesterol level is strictly regulated by our body and additional cholesterol intake from food usually results in only a very small increase of cholesterol in our blood.
If more cholesterol is ingested through food, the body will simply produce less itself.
Saturated fat increases cholesterol
Saturated fat, for example, can lead to an increase in cholesterol levels and it is therefore often recommended to limit its consumption.
This recommendation is based on the assumption that elevated cholesterol levels are harmful to our arteries.
You will find out whether this is the case in the next part of this article.
Summary:
- Cholesterol is vital for human life.
- We need it as a building block for our cell walls, it aids in repair processes and it is the precursor for important hormones and vitamins.
- Cholesterol from food has little effect on our blood cholesterol level.
If we take in more cholesterol through our diet, our body simply produces less of it and vice versa.
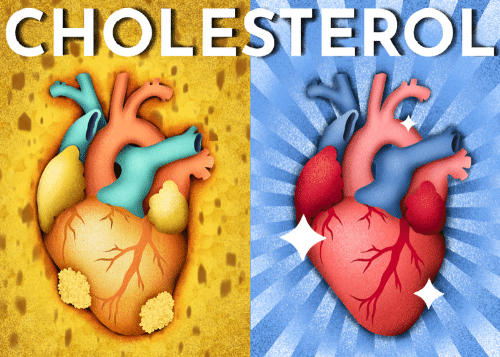
2. Total cholesterol and your heart disease risk
For example, 50% of people who suffer a heart attack have normal cholesterol levels.
At the same time, 50% of the heart-healthy population has elevated cholesterol levels.
Cholesterol-lowering drugs, known as statins, are indeed great at lowering your cholesterol levels, but are disappointingly bad at preventing heart attacks in people who do not yet have existing heart disease.
Statins also frequently have strong side effects that can severely restrict the quality of life of the affected patients.
Low cholesterol is not always better
Some studies suggest that a low total cholesterol level can actually increase the risk of getting certain diseases like cancer or having a stroke.
Particularly in the elderly population (i.e. in those people most at risk for heart disease), a higher cholesterol level is even associated with a lower mortality rate.
It appears that older people with higher cholesterol levels actually live longer and healthier lives than their low cholesterol peers.
Summary:
- Total cholesterol is a fairly meaningless risk factor for heart disease.
- A low cholesterol level may even be associated with negative health consequences.
3. HDL and LDL – “Good” and “bad” cholesterol?
When people talk about “good” or “bad” cholesterol, they are usually talking about the transporter proteins of cholesterol.
Cholesterol is a fat-like substance, which means that it cannot circulate in our watery bloodstream, as fat and water repel each other.
The solution is a system of “water-friendly” transporter proteins that can distribute cholesterol and so-called triglycerides (fats) throughout our body.
These transporter proteins are called lipoproteins and they are categorized into specific types according to their size and density.
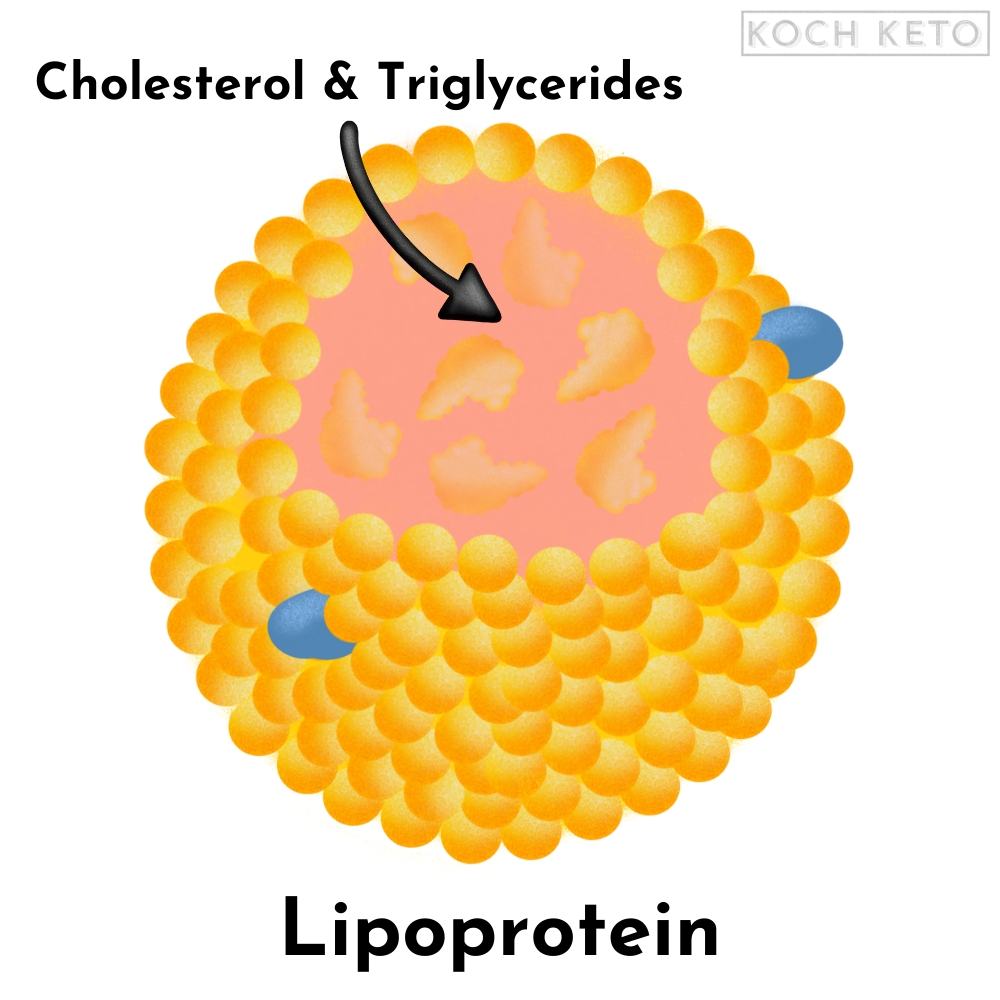
HDL and LDL are abbreviations for the two most well known types of lipoproteins: High-Density-Lipoprotein and Low-Density-Lipoprotein.
While HDL is usually considered to be ” good ” and beneficial for heart health, LDL is usually considered ” bad ” and pathogenic.
Both LDL and HDL transport cholesterol and triglycerides throughout the body and differ not only in terms of density but also in function.
The functions of LDL
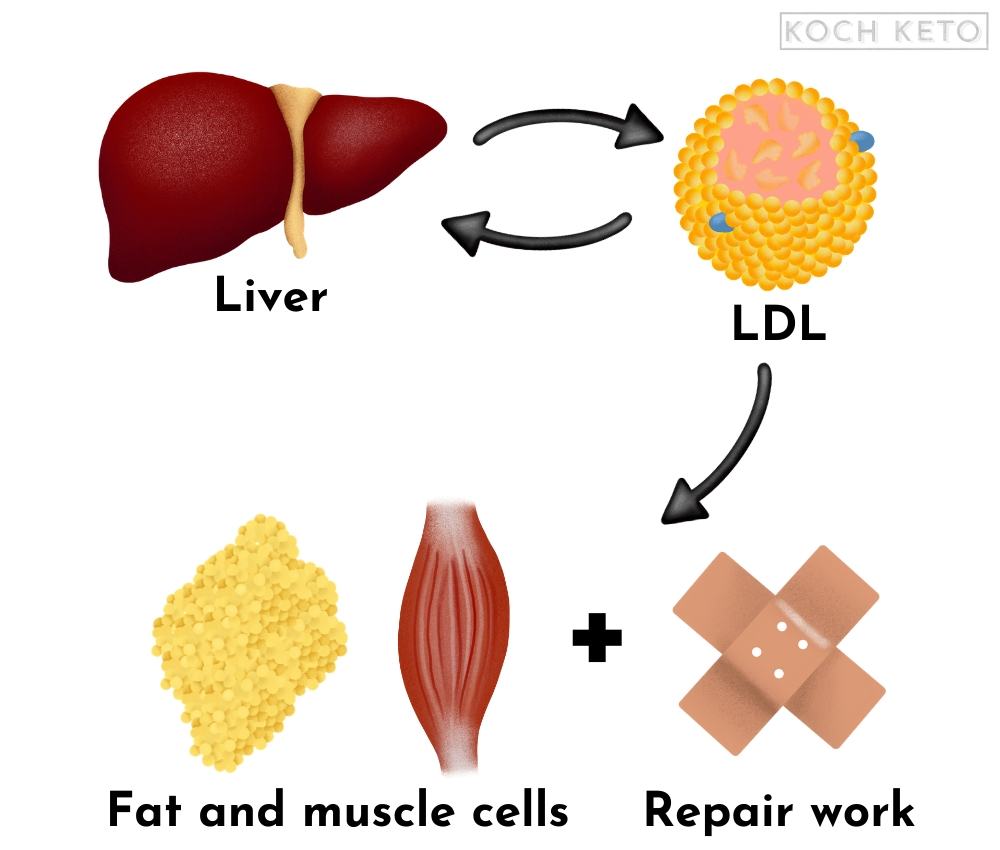
LDL carries cholesterol and triglycerides from the liver to muscle cells and fat cells in our body.
LDL also transports cholesterol to areas in the body where it is needed, for example to injured tissue so it can aid in repair work there.
After some time, the LDL particles are reabsorbed by the liver and recycled.
The functions of HDL
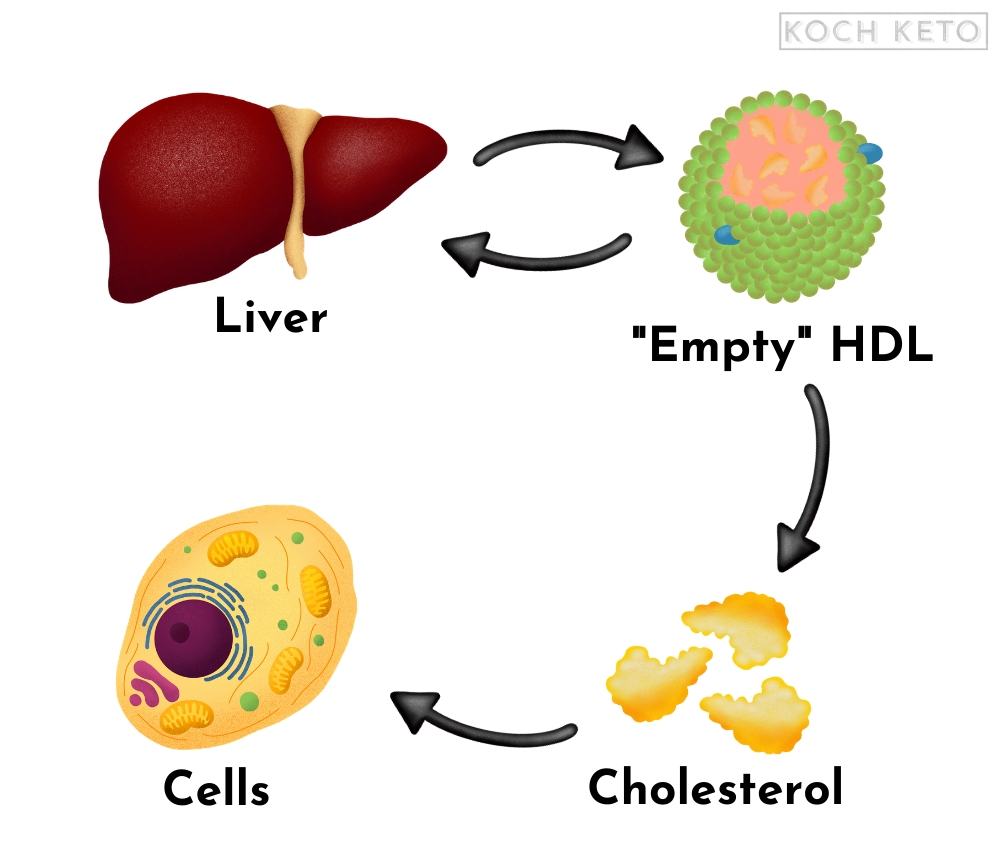
While LDL transports cholesterol and triglycerides from the liver to other parts of the body, HDL basically has the opposite purpose.
It “collects” cholesterol throughout our body and transports it to cells that cannot produce their own cholesterol.
HDL can even reabsorb cholesterol that has entered the arterial walls and can thereby help to reduce cholesterol build-up inside of them.
It also acts as a “control unit” and ensures that our lipid metabolism remains in balance.
HDL is also reabsorbed and recycled by the liver.
The problem with LDL
However, under certain conditions, harmful subtypes of LDL can form:
Small-Dense LDL (sdLDL) and Oxidized LDL (oxLDL).
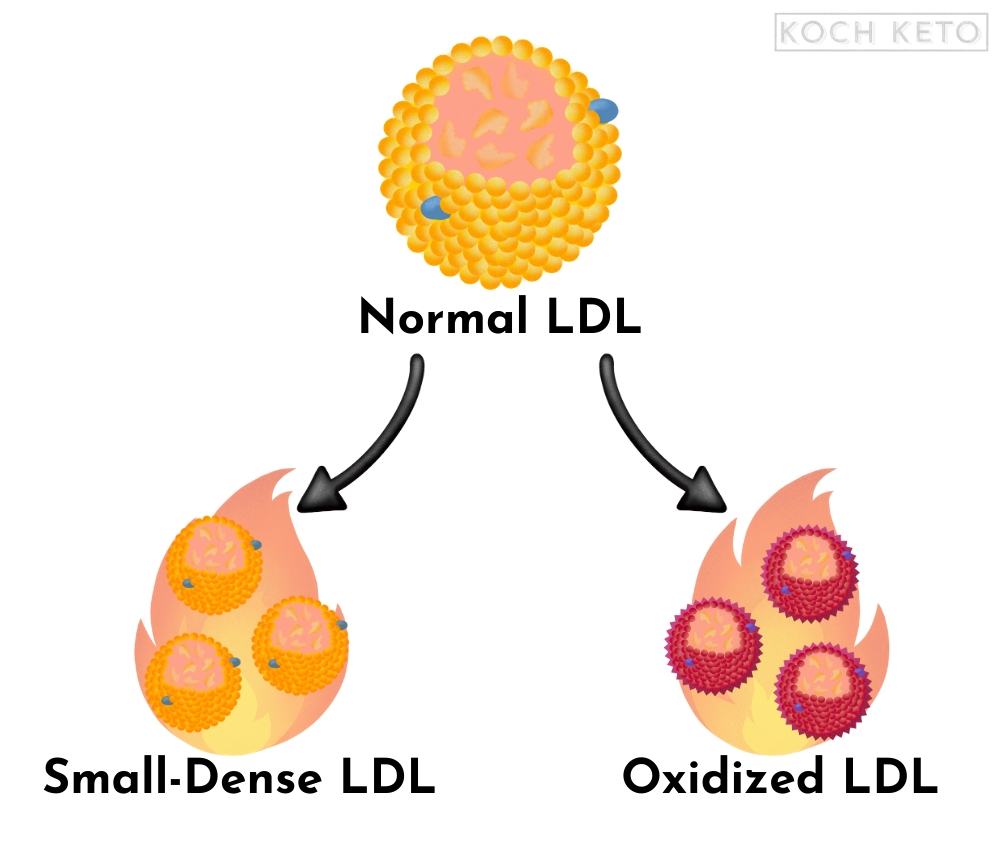
Small-Dense LDL (sdLDL)
It is strongly linked to other known risk factors for heart disease and appears to be much more problematic than larger LDL particles.
It seems that the different sizes and densities of lipoproteins have differing implications for the development of cardiovascular disease.
Oxidized LDL (oxLDL)
Oxidized LDL is even more harmful than sdLDL, because it is not only small and “heavy”, it has also been damaged by the reaction with oxygen (oxidation).
The oxidized LDL particles have an altered structure and are therefore not as readily reabsorbed and recycled by the liver.
As a result, the damaged particles remain longer in the bloodstream, where they can damage the artery walls and contribute to inflammation in the body.
But what causes the formation of these harmful subtypes of LDL?
Summary:
- Cholesterol is unable to circulate in the watery bloodstream by itself and therefore has to be transported by so-called lipoproteins.
- LDL carries cholesterol from the liver to muscle cells, fat cells, and injured areas, while HDL “picks up” cholesterol and takes it to cells that cannot produce their own cholesterol.
- LDL can give rise to two harmful subtypes, sdLDL and oxLDL, which can both contribute to the development of cardiovascular disease.
4. The true origins of heart disease
In the past, the image of clogged kitchen pipes was commonly used as an analogy to how cholesterol might clog up our arteries.
If you pour too much grease into the drain of a kitchen sink, it can quickly become clogged.
Our cardiovascular system also consists of thin “pipes” and the mental image that fat has the same clogging effect in our human “pipe system” was very striking.
In fact, the analogy was so impressive that it was quickly considered a fact, not a theory.
However, having a powerful mental image is not the same as being right and the actual process is much more complex.
How our arteries actually “clog”
The artery itself is a busy place, filled with many blood components such as red blood cells that transport oxygen and lipoproteins that transport cholesterol.
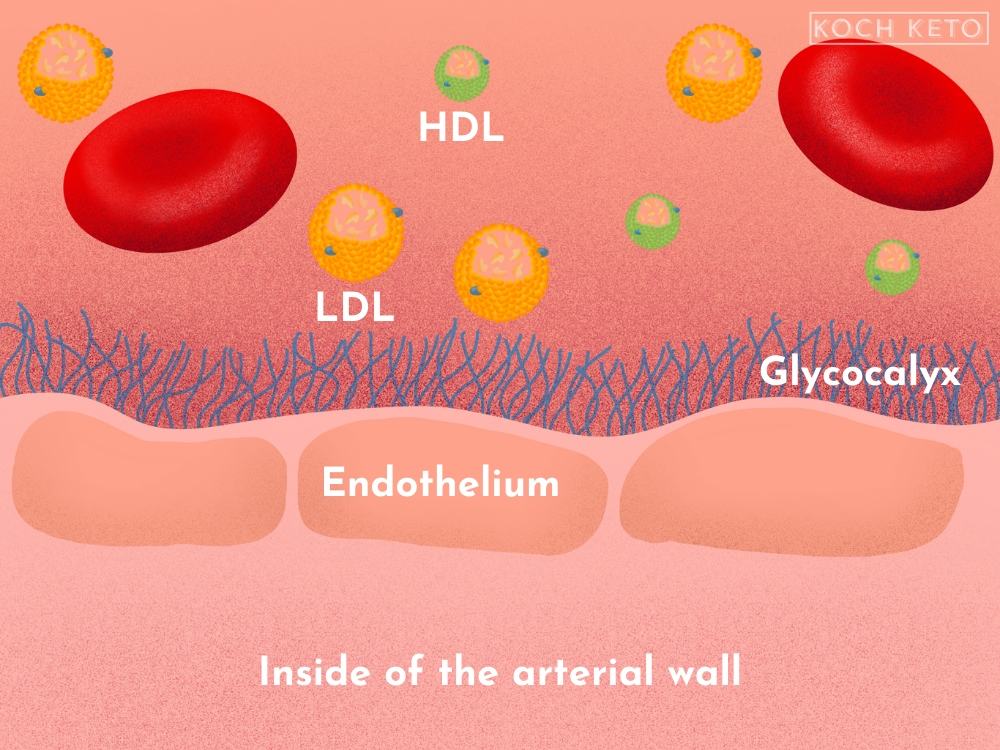
The arterial wall consists of a single layer of cells, the endothelium.
The endothelium is a relatively fragile structure and can be rapidly damaged by inflammatory processes.
When this happens, our body sends cholesterol to the injured areas so it can help aid in the repair process.
At this point, the most problematic LDL particles (sdLDL and oxLDL), as well as the cholesterol they contain, can enter the arterial wall.
There, they can accumulate and trigger further inflammatory processes.
Our body receives the signals of inflammation and will then attempt to stop it, by sending specific immune cells to the inflammation in the arterial wall.
These immune cells absorb the trapped LDL particles as well as the cholesterol they contain.
This results in the formation of so-called “foam cells”, which now gradually form deposits within the arterial wall.
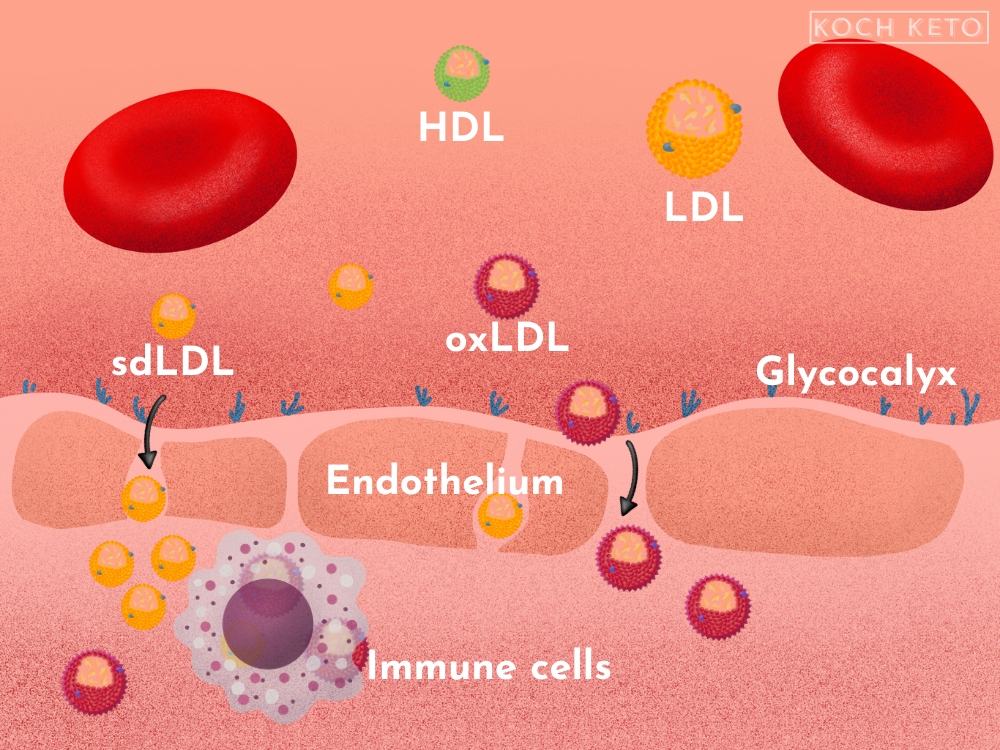
The deposits start to constrict the arteries and can lead to the formation of blood clots, which can, in turn, cut off the oxygen supply to important organs such as the heart.
A heart attack can be the result.
Cholesterol: Arsonist or fireman?
Just like a fireman being called to extinguish fires who always ends up at the site of a fire.
Nobody would think of calling a fireman an arsonist just because he always ends up at the site of a fire.
Yet this is exactly what we do with cholesterol.
Cholesterol is not an arsonist but our in-house firefighter who tries to put out the fires in our arteries.
The starting point for the formation of plaque in our arteries is not cholesterol itself, but inflammatory processes that have damaged the arterial wall.
Cholesterol simply ends up where it is needed.
Cholesterol is not the cause of the build-up of plaque in our arteries, but simply a component of it.
Insulin and high blood sugar – the true arsonists
However, if a high level of LDL particles is paired with a high level of insulin, the risk will skyrocket.
It seems as though LDL is harmful mainly in combination with increased blood sugar and insulin levels.
High blood sugar and insulin disrupt our protective mechanisms
There are several protective mechanisms to ensure that harmful particles like oxLDL cannot penetrate the inside of the arterial wall.
The first and perhaps most important protective mechanism is a thin layer of carbohydrates and proteins covering the endothelium, called the glycocalyx.
The glycocalyx functions like a sieve and is the first line of defense to prevent unwanted particles from entering into the arterial wall.
This thin and fragile layer can be easily damaged by known risk factors for heart disease like smoking and high blood pressure.
But there are other factors that can damage it as well, most notably: a high blood sugar level.
A high carbohydrate meal virtually dissolves our critical protective layer.
The cell layer underneath, our endothelium, is left exposed and is now much more likely to be damaged and susceptible to inflammatory processes.
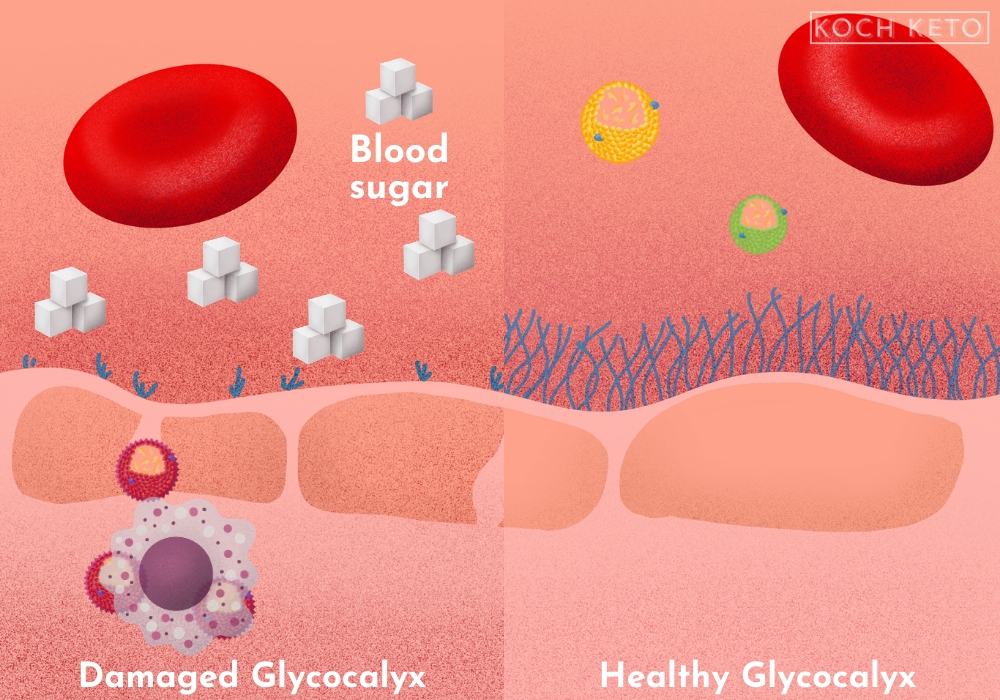
It takes up to 12 hours for the glycocalyx to recover from a very high-carbohydrate meal, but due to our modern eating habits it never even gets the chance.
After 3-4 hours we usually munch on our next high carbohydrate meal or snack, thereby undoing the slight recovery of our glycocalyx.
If the first line of defense does no longer work, harmful particles such as oxidized LDL can pass through the underlying cell layer and build up inside of our artery walls.
If the remaining protective mechanisms within the arterial wall also fail, deposits build up and heart disease develops.
Summary:
- The first step in the development of cardiovascular disease is inflammatory processes in the arteries, not cholesterol simply “clogging up” our arteries.
- Cholesterol is sent to the site of “injury” in the artery due to its natural role in repair processes, where under certain circumstances it can enter the damaged arterial wall.
- Once cholesterol enters the arterial wall, it can trigger further inflammatory processes which over time can lead to the build-up of deposits and cause a heart attack.
- A high level of LDL alone carries only a slightly increased risk of dying from heart disease – but in combination with other risk factors such as high blood sugar or insulin levels, the risk increases greatly.
- Known risk factors such as smoking, high blood pressure, and high blood sugar and insulin levels switch off our body’s protective mechanisms within our arteries and enable harmful sdLDL and oxLDL particles to enter the arterial wall.
5. The most relevant risk factors for heart disease
The disease remains “invisible”.
A coronary artery calcium scoring, or CAC scan, can visualize the existing calcification in your arteries and thus provide the most accurate picture of your heart health.
Thanks to a CAC scan, you no longer have to calculate your odds of having heart disease by using relatively unreliable risk markers, but instead, you get a clear picture of how your heart is doing.
It is unmatched in terms of accuracy and outshines conventional risk factors like total cholesterol.
There are however a few risk factors that may not come close to the calcium score in terms of accuracy and predictable value but are still significantly better than the total cholesterol level.
The risk factors
1. Unfavorable ratio of LDL/HDL and triglycerides/HDL
High LDL and high triglycerides paired with low HDL indicate that our fragile lipid metabolism is not functioning properly and the ratio of these particles to one another is much more meaningful than any of the markers alone.
An unfavorable ratio of HDL/triglycerides is also a relatively good marker of insulin resistance (basically the early stage of type 2 diabetes).
An unfavorable ratio is also an indication that there is a higher number of oxLDL and sdLDL particles, instead of “normal” LDL.
2. Number of sdLDL and oxLDL particles
3. High insulin level or insulin resistance/type 2 diabetes
4. High blood sugar & HbA1C
The HbA1C reading represents the reaction of our red blood cells with sugar (called glycation): A high value is a bad sign.
Unlike conventional risk factors like your total cholesterol level, a calcium score, and the risk factors mentioned above can give you a fairly accurate picture of your heart health.
Summary:
- A calcium scoring of the arteries, or CAC scan, can provide a fairly accurate picture of the condition of your cardiovascular system and outshines conventional risk markers.
- The best risk markers for heart disease are not, as often assumed, the total cholesterol value or the LDL value, but certain ratios of blood components to one another.
- For example, a high level of LDL is a relatively unreliable marker when at the same time, triglycerides are low and HDL is high.
6. How the ketogenic diet affects the most relevant risk factors
According to the conventional theory, the most relevant risk factors mentioned in the previous section should worsen significantly with a high-fat diet.
However, dozens of studies show exactly the opposite.
A ketogenic diet improves the most relevant risk factors – even without calorie restriction and better than low-fat diets.
Better HDL/triglyceride and HDL/LDL ratio
A good ratio of these values to each other indicates low insulin resistance and a well-balanced lipid metabolism.
Following a ketogenic diet consistently increases HDL levels and decreases triglyceride levels.
The LDL level often remains the same or increases slightly, resulting in a better HDL/LDL ratio due to the increase in HDL.
LDL remains the same or increases slightly
The LDL level is only marginally affected by low carb diets – it will either remain the same or increase slightly.
If the LDL level does increase, it is most likely not an increase of the harmful sdLDL particles, but of the more harmless, larger LDL particles.
In the context of a low carb, high fat diet, an increase in LDL actually makes sense too, as the main function of LDL is to transport cholesterol and tryglycerides from the liver to muscle and fat cells.
If we eat more fat, more fat must be transported within our body and an increase in the transporters for fat seems a logical consequence.
A further indication that the increase in LDL in the context of a low carb diet seems to be not pathological, but a normal consequence of our fat metabolism is that LDL usually also increases during prolonged fasting.
During fasting, our body fat is broken down to serve as an energy source and consequently more fat is transported in the blood.
Calorie restriction not necessary for positive effects
However, the positive effects of the ketogenic diet on the most relevant risk factors for heart disease can be seen even without any calorie restriction.
Even if their weight is held constant, people who follow a ketogenic diet will usually see positive changes in their risk factors.
This makes a low carb diet even more effective than a low-fat diet, as the positive effects seen with low-fat diets are usually tied to calorie restriction, which can never be maintained forever.
Reducing carbohydrate has dose-dependent positive effects
But that’s not all, the positive effects seem to be dose-dependent as well.
In other words, the more you restrict the carbohydrates you eat, the more beneficial are the effects.
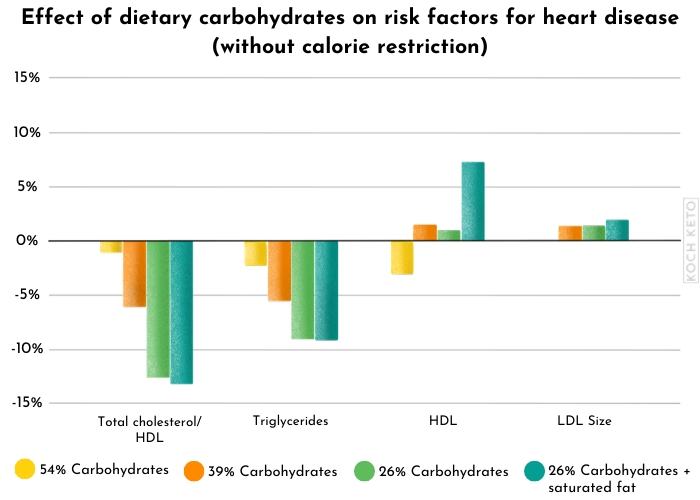
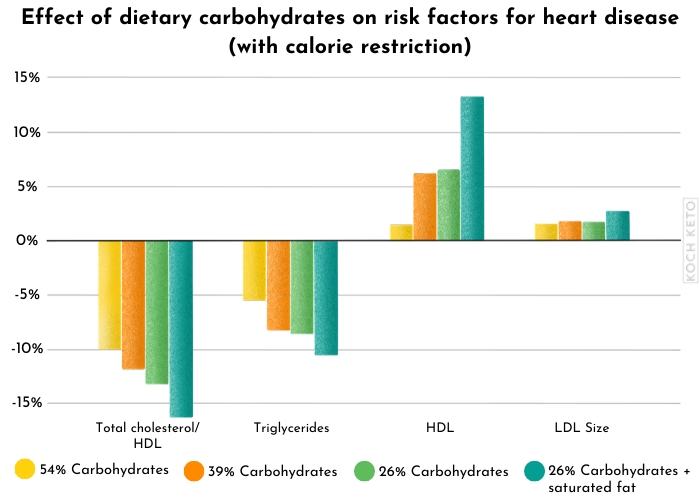
A large body of scientific evidence indicates that a low carb diet is a good idea if you want to improve the most relevant risk factors for heart disease.
Summary:
- Low carb diets have a positive effect on the most relevant risk factors for heart disease.
FAQ’s
Will the keto diet increase my cholesterol level?
In addition, if cholesterol increases on a ketogenic diet, it is usually accompanied by other positive changes in the lipid metabolism, such as a decrease in triglycerides and an increase in HDL.
What will happen to my LDL level on the ketogenic diet?
However, the most harmful subtypes of LDL (sdLDL and oxLDL) usually do not increase or may even decrease.
Why is LDL "bad" and HDL "good"?
For this reason, it often ends up within the arterial walls and is thus associated with the development of heart disease.
HDL basically has the opposite job and can remove cholesterol from the arterial walls and therefore has a negative association with heart disease.
Can I eat low carb if I have high cholesterol?
Nevertheless, you should always consult your doctor before making any major changes in your diet.